
Thromboembolism-risk-based algorithm decreases anticoagulation rates and bleeding risk after liver transplantation
Fidel Lopez-Verdugo1, Spencer LeCorchick1, Jorge Sanchez-Garcia1, Sean Dow1, Jake Krong1, Gordon Harmston1, Mark E. Boschert1, Ivan Zendejas1, Edward J. Frech1, Andrew I. Gagnon1, Robert Jones1, Shiro Fujita1, Richard K. Gilroy1, Manuel I. Rodriguez-Davalos1, Scott M. Stevens2, Scott C. Woller2, Diane Alonso1.
1Transplant Services, Intermountain Medical Center, Salt Lake City, UT, United States; 2Thrombosis Clinic, Intermountain Medical Center, Salt Lake City, UT, United States
Introduction: There is scarce literature providing clinical guidance on deep vein thrombosis (DVT) management after liver transplantation (LT), where hemostatic disturbances are constantly changing as the synthetic capacity of the liver increases. We hypothesized that an anticoagulation algorithm based on thromboembolism risk would decrease anticoagulation rates and bleeding risk after LT.
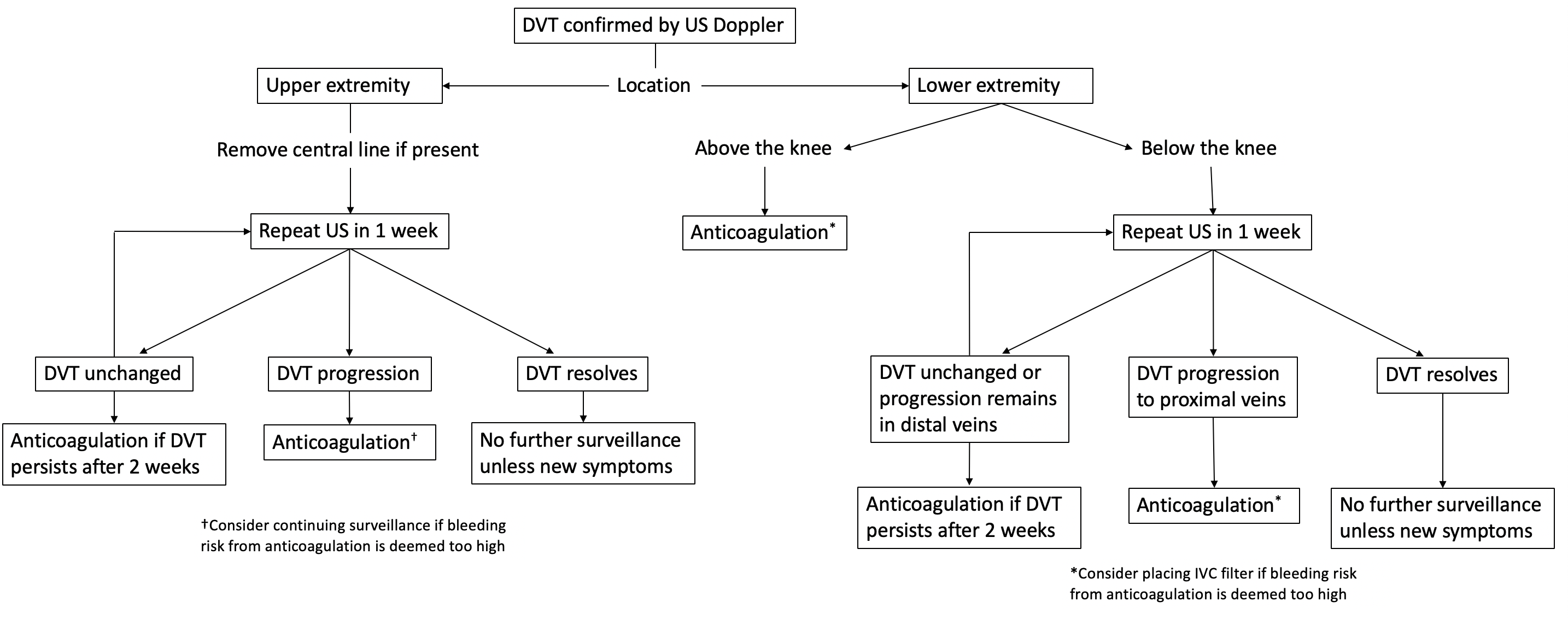
Materials and Methods: Ambispective, single center study. An algorithm for management of DVT after LT was developed based on thromboembolism risk according to DVT location.
Data from patients who received a LT before implementation of the algorithm (control group: 2017) was collected retrospectively, and patients who received a LT during implementation of the algorithm (study group: 2018-2019) were followed prospectively. Primary endpoints included anticoagulation after diagnosis of DVT and bleeding (drop in hemoglobin ≥ 2 g/dL or transfusion of ≥2 units of blood). Safety outcomes included death, pulmonary embolism, return to OR and readmission within 30 days of LT. Univariate logistic regression analysis was performed to evaluate if implementation of the algorithm was associated with decreased odds of anticoagulation and bleeding, and to assess possible confounders.
Results and Discussion: The study and control groups included 90 and 50 patients, respectively. There were no baseline differences on gender, age, or history of portal vein thrombosis, DVT or hypercoagulability disorders between groups.
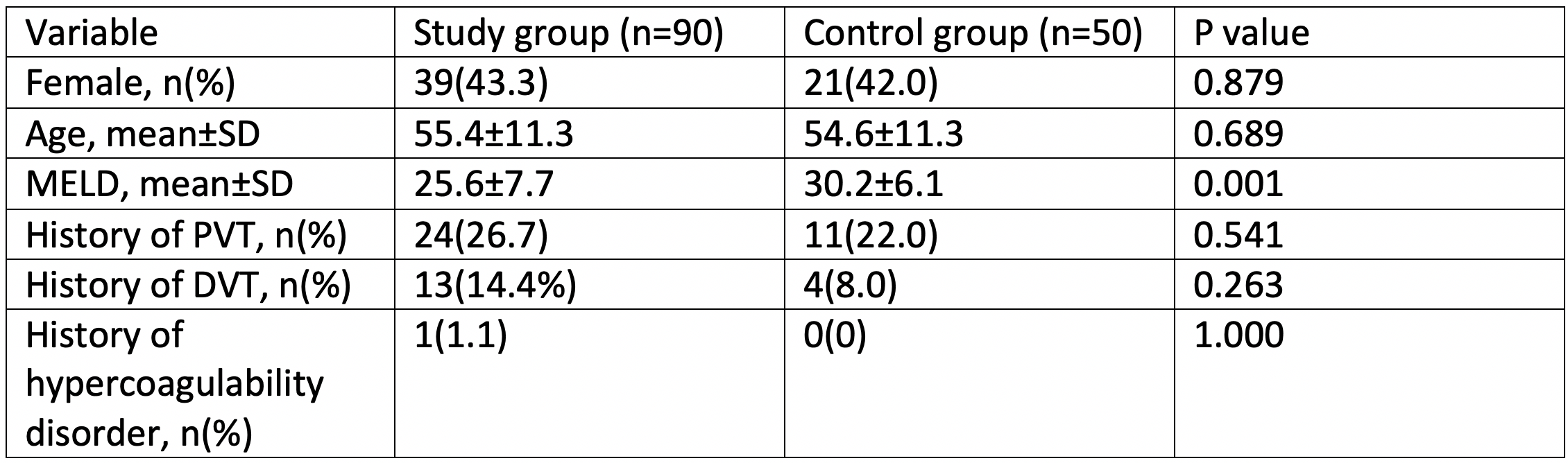
The study group had lower MELD scores. 16 (17.8%) patients from the study group and 5 (10%) controls developed DVT within 14 days (p=0.217). Of these, 2 (12.5%) study group and 4 (80%) control group patients received initial anticoagulation after DVT diagnosis (p=0.011). The study group had decreased odds of receiving initial anticoagulation after DVT (OR = 0.036, 95% CI: 0.003-0.503; p=0.014), and a tendency of decreased risk of bleeding (OR = 0.154, 95% CI: 0.017-1.369; p=0.093) compared to the historical cohort. MELD scores did not appear to have a significant association with DVT (OR = 1.023, 95% CI: 0.961-1.090; p=0.478), initial anticoagulation (OR = 1.089, 95% CI: 0.939-1.262; p=0.258), or bleeding (OR = 1.012, 95% CI: 0.882-1.162; p=0.860). No significant differences were observed on death, pulmonary embolism, return to OR and readmission within 30 days between groups.
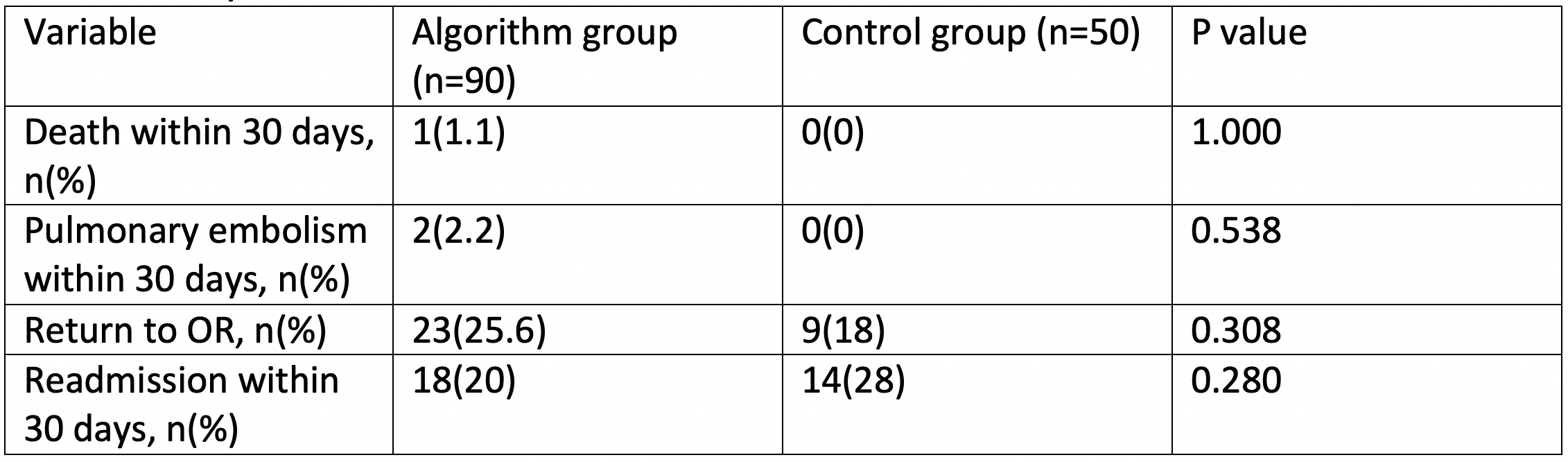
Conclusion: Implementation of a thromboembolism-risk-based algorithm for the management of DVT after LT decreases anticoagulation rates and may decrease bleeding risk. Use of this algorithm resulted in an increase of observation and US Doppler follow up. However, this increased surveillance balances favorably against the continuous laboratory monitoring and increased risk of bleeding associated with routine anticoagulation. Implementation of this algorithm does not seem to increase the rate of adverse events related to thromboembolism
[1] Blasi A, Hernandez V, Fernandez J, et al. Venous Thrombotic Events After Liver Transplantation. Clin Appl Thromb Hemost. 2018;24(2):317–322. doi:10.1177/1076029616680477
[2] Northup P, Reutemann B. Management of Coagulation and Anticoagulation in Liver Transplantation Candidates. Liver Transpl. 2018;24(8):1119–1132. doi:10.1002/lt.25198
[3] Emuakhagbon V, Philips P, Agopian V, Kaldas FM, Jones CM. Incidence and risk factors for deep venous thrombosis and pulmonary embolus after liver transplantation. Am J Surg. 2016;211(4):768–771. doi:10.1016/j.amjsurg.2015.11.028
There are no comments yet...