Combined heart-liver transplantation: Single center experience
Amit Sharma1, Angela Sickels1, Brianna Ruch1, Adrian Cotterell1, Chandra Bhati1, David Bruno1, Vinay Kumaran1, Aamir Khan1, Seung D. Lee1, Mohammad S. Siddiqui1, Richard Stravitz1, Marlon Levy1, Keyur Shah2, Vigneshwar Kasirajan2.
1Hume-Lee Transplant Center, Virginia Commonwealth University, Richmond, VA, United States; 2Pauley Heart Center, Virginia Commonwealth University, Richmond, VA, United States
Introduction: Combined heart-liver transplantation (CHLT) remains the only curative option for patients with coincident end-stage heart and liver disease. Due to the complexity and logistics of the procedures, very few centers perform CHLT worldwide. We report our single center outcomes after CHLT.
Methods: Retrospective analysis of all CHLT performed at our center between 09/2013 to 12/2019 was done. Continuous variables are expressed using mean (± standard deviation) or median (range). Categorical variables are presented as counts and proportions.
Results and Discussion: Six CHLT were performed. One patient with heart-liver-kidney transplant was excluded from this analysis. Most brain dead donors were young males (29 ± 12.29 years).
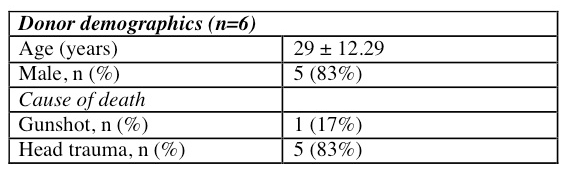
The average age of the recipients was 55 ± 5.62 years. The indication for heart and liver transplant in 5/6 patients was familial amyloidosis. Two patients shared the Val122Ile mutation, which is found in greater frequency in the African American population. The indication in one patient was non-ischemic cardiomyopathy (NICM) with concomitant hepatitis C cirrhosis. Three patients (50%) had at least one prior sternotomy. Two patients were bridged to transplant with TAH. Other mechanical support included one patient with each HMII and IABP. One patient required inotropic support prior to transplant. The recipient LVEF at the time of transplant was 25 ± 7.38%. The average MELD score at transplant was 17.17 ± 3.76.
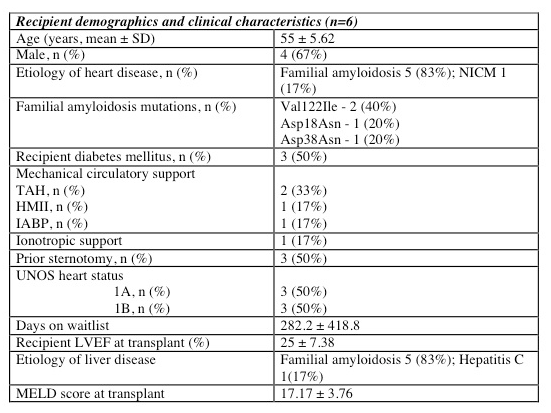
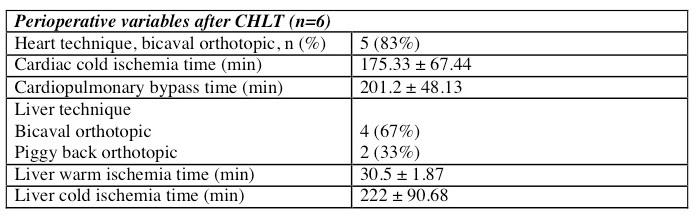
The mean cold ischemic time was 175.33 ± 67.44 min for heart and 222 ± 90.68 min for liver. Average cardiopulmonary bypass time was 201.2 ± 48.13 min. Two of the explanted livers were utilized for domino transplantation while liver fibrosis due to passive cogestion on histopathology precluded their use in others. A majority of cardiac transplants occurred using a bicaval orthotopic technique (83%. Bicaval technique was used for liver transplant in 67% of patients.
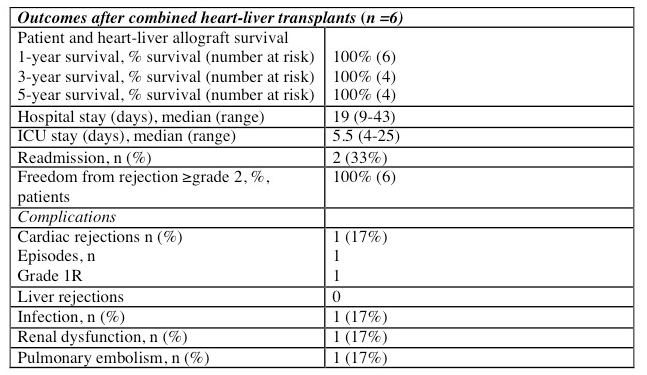
The median intensive care (ICU) and hospital stays were 5.5 and 19 days respectively. One patient had post-operative renal dysfunction requiring dialysis and another developed a retroperitoneal abscess requiring operative drainage. One patient developed a right-sided PE, which resolved with apixaban. One patient experienced grade 1R cardiac rejection, which resolved with high dose methylprednisolone. Patient and graft survival for both organs was 100%.
Conclusions: Familial amyloidosis was the indication for combined heart-liver transplantation in a majority of our recipients. Combined heart-liver transplantation for familial amyloidosis achieves excellent outcomes in selected patients with very few complications. The possible use of livers explanted from patients with familial amyloidosis for domino liver transplantation can contribute to the liver donor pool and thus help justify the simultaneous allocation of two organs to one recipient.
There are no comments yet...