Opioid use prior to liver transplant is associated with increased risk of death after transplant
Hillary Braun1, Marisa P. Schwab1, Chengshi Jin2, Dominic Amara3, Trevor Grace4, Rhiannon Croci5, Chris E. Freise1, John P. Roberts1, Neil Mehta6, Ryutaro Hirose1, Nancy L. Ascher1.
1Department of Surgery, University of California, San Francisco, San Francisco, CA, United States; 2Department of Epidemiology and Biostatistics, University of California, San Francisco, San Francisco, CA, United States; 3School of Medicine, University of California, San Francisco, San Francisco, CA, United States; 4Department of Orthopedic Surgery, University of California, San Francisco, San Francisco, CA, United States; 5Health Informatics, University of California, San Francisco, San Francisco, CA, United States; 6Department of Medicine, University of California, San Francisco, San Francisco, CA, United States
Background: The impact of the opioid epidemic on liver transplant (LT) candidates and recipients has not been widely studied, but pre-transplant opioid use has been associated with inferior post-transplant outcomes. The purpose of this study was to determine whether prior opioid use impacted post-LT opioid use, graft survival, or patient survival.
Materials and Methods: A retrospective review of all primary adult LT recipients at our institution between 2012-2019 was performed. Descriptive statistics were stratified according to opioid use prior to transplant. UV and MV regression models were used to identify predictors of oral morphine equivalents (OME) at discharge (DC), days of opioids prescribed, and post-LT refills. Survival was evaluated with Cox proportional hazards models.
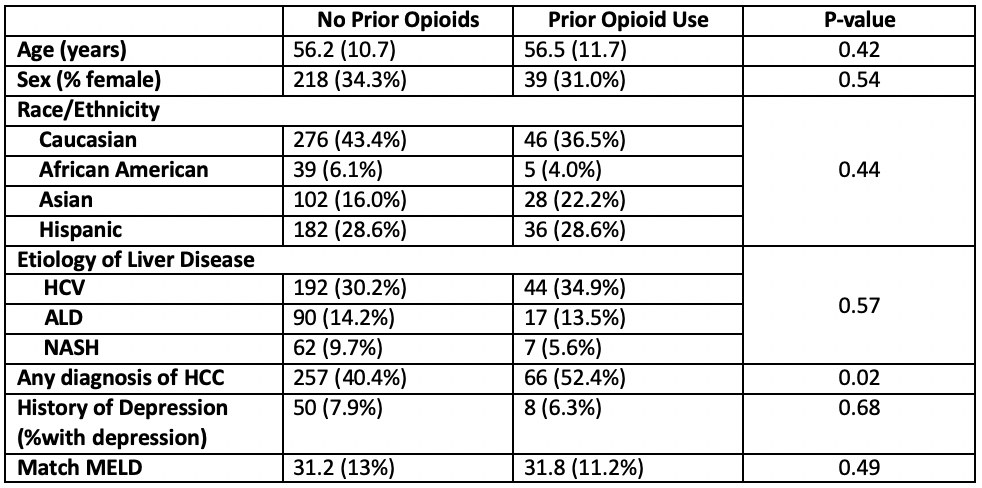
Results: 762 patients were included, of whom 126 (16.5%) had a history of opioid use prior to LT. The only significant demographic difference was a greater incidence of HCC in the cohort of patients with opioid use prior to LT (52.4% vs. 40.4%, p=0.02, Table). Patients with prior opioid use had higher OME the day prior to DC (55.8 vs. 32.9, p=0.03), greater total OME prescribed at DC (456 vs. 317, p=0.01), and more refills 30-60 days after LT (29.4% vs. 19.7%, p=0.02). At 60-90 days post-transplant, 10.7% of opioid naïve patients and 13.5% of prior opioid patients required refills.
In MV modeling, longer post-operative length of stay, prior opioid status, and greater OME on the day prior to DC were associated with total OME at DC.
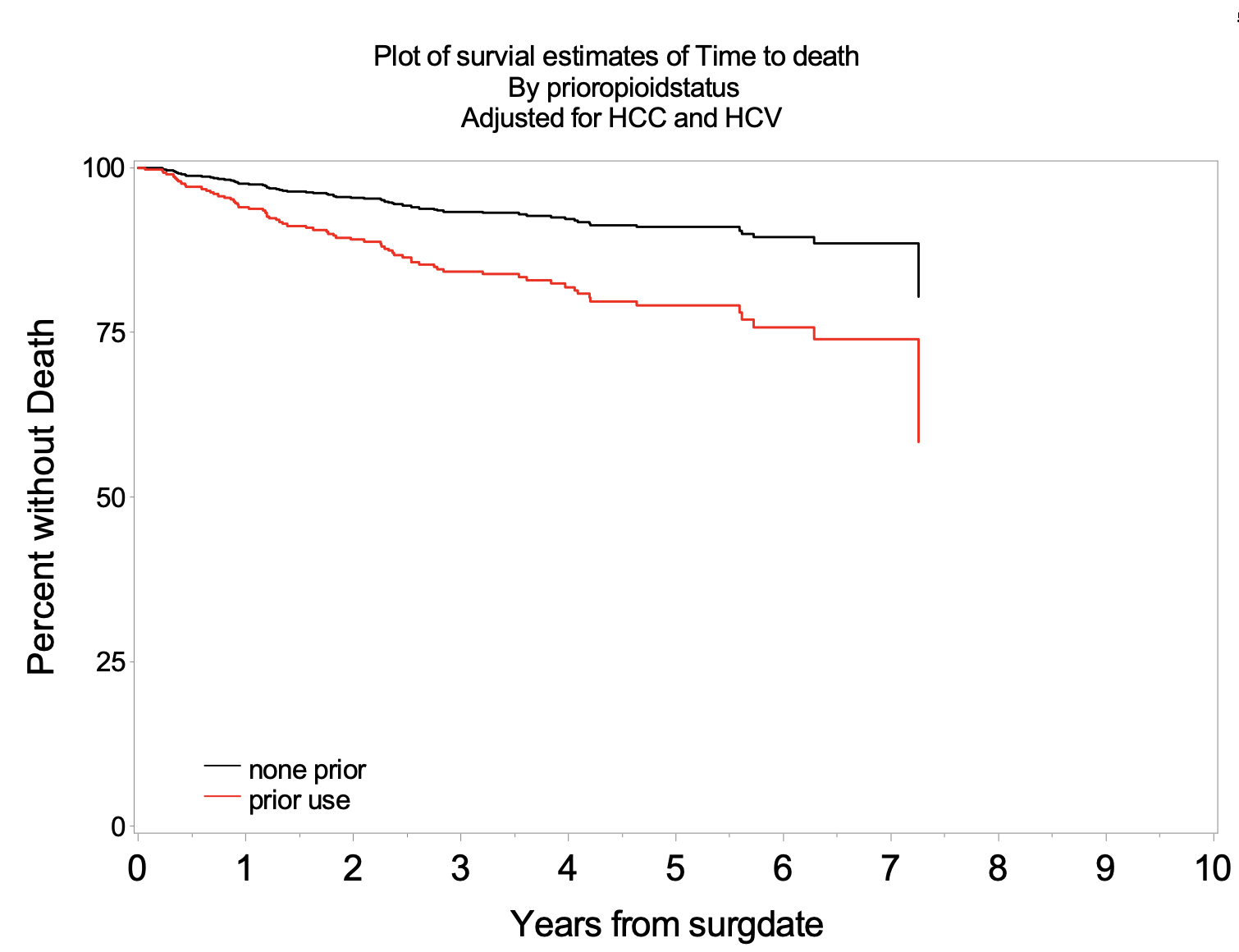
There was no difference in graft survival, however patient survival was significantly worse in patients with an opioid history prior to LT (p<0.001) which remained significant after adjusting for both HCV and HCC (Figure, p=0.046).
Discussion: The cohort of patients with opioid use prior to LT had a higher proportion of patients with HCC, so it is possible that opioid use is associated with procedures aimed at tumor management and downstaging. However, opioid use prior to LT is associated with increased risk of death after LT, even after adjusting for HCC and HCV.
Conclusions: Approximately 16% of patients have a history of opioid use prior to LT, and a diagnosis of HCC is more prevalent in this population. Opioid use prior to LT is associated with increased risk of death following transplant.
CJ is part of the Biostatistics Core that is generously supported by the UCSF Department of Surgery..
