Lower extremity vascular complications after simultaneous pancreas kidney transplant
Hillary Braun1, Dominic Amara2, Amy M. Shui3, Thomas Sorrentino1, Joel L. Ramirez1, Joseph Lin1, Anna Mello1, Peter G. Stock1, Jade S. Hiramoto1.
1Department of Surgery, University of California, San Francisco, San Francisco, CA, United States; 2School of Medicine, University of California, San Francisco, San Francisco, CA, United States; 3Department of Epidemiology and Biostatistics, University of California, San Francisco, San Francisco, CA, United States
Introduction: Type 1 diabetes mellitus (DM) is the leading indication for simultaneous pancreas kidney transplantation (SPK). Prior work has demonstrated a 2% incidence of lower extremity (LE) vascular complications in kidney recipients, and a 5-23% incidence in SPK recipients, yet there is no standard vascular evaluation or follow up for these patients. The purpose of this study was to describe the incidence and risk factors for LE vascular complications following SPK at a single United States transplant center.
Methods: A retrospective review of all patients who underwent SPK at our institution between 2000-2019 was performed. Patients were excluded for age<18 or prior pancreas transplant. Baseline demographics, comorbidities, transplant details, medications, and vascular complication data were collected from the electronic medical record, and tested for differences by LE intervention status using t-tests and Fisher’s exact tests. Graphs of the Kaplan-Meier survival estimates, along with Cox proportional hazards regression models, were used to determine the effect of various risk factors on the need for LE intervention after SPK. Significance was set at 0.05.
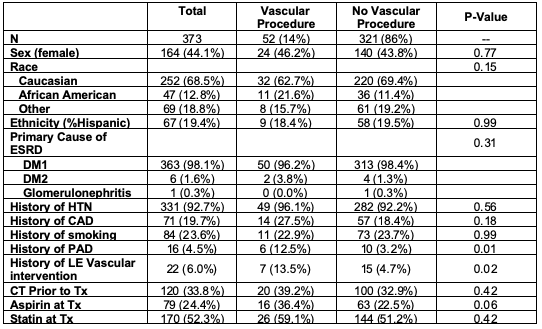
Results: 373 patients were included, of whom 52 (14%) required at least one LE intervention following SPK (Table). A total of 75 interventions were performed in this cohort: 16 endoluminal revascularization procedures, 2 open bypass grafts, 36 amputations, and 21 podiatry procedures. Only 3 patients (0.8%) had pre-transplant ankle brachial indices (ABIs).
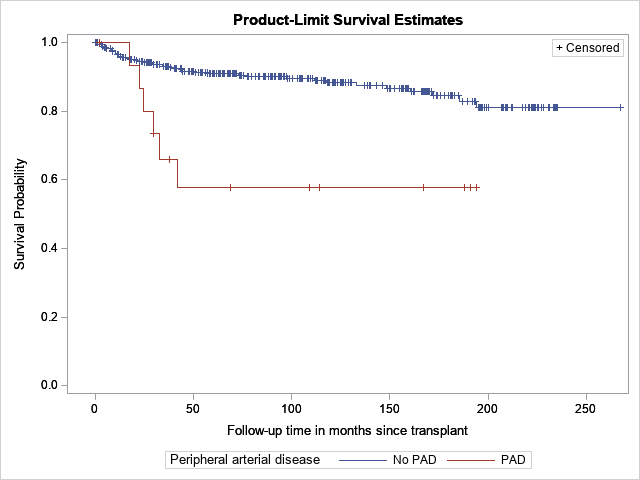
Compared with white patients, African American patients were significantly more likely to undergo LE vascular intervention after SPK (HR 2.54 CI 1.26-5.10, p=0.01). Patients with a prior LE vascular intervention (HR 4.42, CI 1.96-9.96, p<0.001) or previous diagnosis of PAD (HR 3.80, CI 1.60-8.99, p=0.002, Figure) were also significantly more likely to require intervention after SPK compared with patients who had no prior history of vascular interventions and no documented PAD, respectively. In a MV model including the risk factors of diabetes, dialysis, race and PAD, PAD remained significantly associated with LE vascular intervention after SPK (HR 3.39 95% CI 1.36-8.21, p=0.01).
Discussion: LE vascular complications after SPK are a major source of morbidity. In our population, 14% of SPK recipients required a LE vascular intervention after transplant and only 3 patients (0.8%) had pre-operative ABIs. Pre-operative non-invasive arterial evaluation may help to identify SPK recipients at high risk for LE vascular complications and prompt close follow-up with a vascular provider.
Conclusion: Fourteen percent of SPK patients required one or more LE vascular interventions after SPK. African American patients, and those patients with a history of PAD or prior LE intervention are at particularly high risk for LE vascular events after SPK.
AS is part of the Biostatistics Core that is generously supported by the UCSF Department of Surgery..
There are no comments yet...
